As the European Commission gets set to review the EU’s pharmaceutical legislation, two issues demand particular attention: ensuring supplies of key medicines, especially antibiotics—and encouraging the innovation needed to maintain the therapeutic options available, which come from having new and different antibiotics. Francesca Scassellati Sforzolini, Healthcare & Life Sciences Lead, Europe, reports.
Last winter, Europe experienced what public health officials had long feared: a wave of bacterial infections that couldn’t be treated by antibiotics. As respiratory infections surged across the continent, pharmacies struggled to maintain supplies of key medicines, including antibiotics like amoxicillin.
The good news is that the shortages are lessening and “a lot of those things [that caused the shortage] are solvable, and hopefully will be solved for next year,” Emer Cooke, the head of the European Medicines Agency, said in February.
The bad news: There’s growing consensus that without fundamental changes to Europe’s market framework, the continent is bound to find itself without antibiotics at some point—either because pharmacies’ shelves are again empty, or, more terrifyingly, because they are stocked with antibiotics that don’t work.
The European Commission was set to revise the EU’s pharmaceuticals legislation by the end of 2022, but this has been delayed since, with the last announced date of 29 March likely to be delayed once more. This review is a “once-in-a-generation opportunity … to update a 20-year-old regulatory system and make it fit for purpose for the innovations of the future,” wrote Nathalie Moll, Director General of European Federation of Pharmaceutical Industries and Associations.
Of particular importance are two related but distinct issues: safeguarding the supplies of antibiotics that work today, and encouraging the innovation needed to develop new antibiotics.
The Rise of Antibiotics … and Superbugs
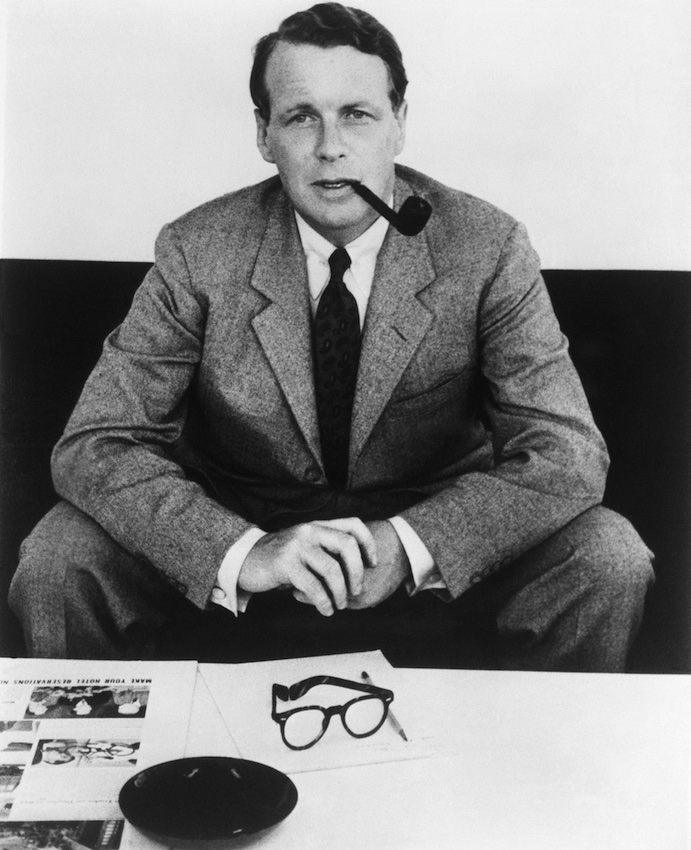
“Antibiotics may be the biggest success story in the history of medicine,” the Wellcome Trust, a global health foundation, argues. Since antibiotics became widely available in the 1940s, global deaths from infectious diseases have plummeted.

Original chart by the Wellcome Trust; data from OECD
Yet, “the great virtue of penicillin—that it scythes its way through all manner of bacteria—is also its elemental weakness,” Bill Bryson wrote in his bestseller The Body. “The more we expose microbes to antibiotics, the more opportunity they have to develop resistance.”
As the use of antibiotics has skyrocketed (see chart 2), resistance to them has grown (see chart 3).

Original chart by the Wellcome Trust; data from PNAS (https://www.pnas.org/doi/10.1073/pnas.1717295115)

Original chart by the Wellcome Trust; data from PNAS (https://www.pnas.org/doi/10.1073/pnas.1717160115)
The sharp rise in antimicrobial resistance (AMR) is now one of the world’s most pressing public-health issues. Drug-resistant infections—often called “superbugs”—now cause more deaths than HIV/AIDS and malaria worldwide. By 2050, according to one estimate, AMR could result in 10 million deaths annually. When not fatal, AMR still leads to “longer hospital stays and higher medical costs,” according to the World Health Organization. “Superbugs” were partly responsible for Europe’s wintertime surge of infections, and are among the leading contenders to cause the next global pandemic.
A Market in Need of Medicine
The solution, according to the Wellcome Trust, is “to use the antibiotics we have sparingly, but we also need to keep developing new ones.” Yet, as Wellcome points out, developing an antibiotic takes between 10 and 15 years and costs more than $1 billion.
Such long timelines and high costs make it all but impossible for startups—in 2019, Achaeogen and Aradigm, two prominent antibiotic startups, went bankrupt. Meanwhile larger companies find it difficult to justify investing in developing a drug that, ideally, will be used as little as possible. There has not been a discovery of a new class of antibiotics since the 1980s.

Original chart by the Wellcome Trust; data from Pew Charitable Trusts
“We need action now to respond to the global health threat caused by AMR,” says David Earnshaw, Associate Vice President, European Public Policy, for MSD [Merck, Sharpe & Dohme], a leading pharmaceutical company. “The market alone doesn’t work when it comes to antimicrobial research. We need new medicines which, in the case of anti-microbials, should only be used very sparingly: hence the market failure.”
According to Andrea Chiarello, Head of EU Government Affairs for Pfizer, that market failure stems from there being “very few incentives for venture capital, small biotechs, or global pharmaceutical companies to invest in antimicrobial R&D. The market potential is limited due to several, co-existing factors: the steep costs of antimicrobial development; the high risk of failure; the traditional HTA [health technology assessment] processes which do not properly recognize the full societal value of antimicrobials; and the need to keep usage at a minimum to ensure stewardship and conserve antimicrobials for use in severe cases of resistance. The best way to convince companies and investors to allocate more capital into this field is for governments to address the challenging commercial environment by prioritizing the incentives needed to reinvigorate R&D.”
A Global Problem, Pronounced in Europe
These problems are not unique to Europe, but they are pronounced on the continent—and, given the European Commission’s looming pharmaceutical review, they are timely.
Challenge 1: Ensuring Supply of Existing Antibiotics and Medicines
To oversimplify, Europe’s shortages were driven by two forces: spiking demand and constrained supply. Seasonal spikes of respiratory infections are normal, but this wave’s peak was exceptionally high. A leading hypothesis: After years of pandemic restrictions, people’s immune systems were weakened.
The constrained supply was caused by a number of familiar forces: inflation, supply-chain kinks, and risings costs. And it’s here policymakers can take steps to help avoid a repeat scenario. One move the European Commission is considering is forcing manufacturers to hold larger reserve supplies of key medicines, including antibiotics. That should help. Yet other challenges remain. For instance, Europe’s market framework does not allow manufacturers to adjust prices to reflect changes in costs. Reuters reported electricity prices had climbed 10-fold for some drugmakers since Russia’s invasion of Ukraine, while raw materials costs had soared by as much as 160%.

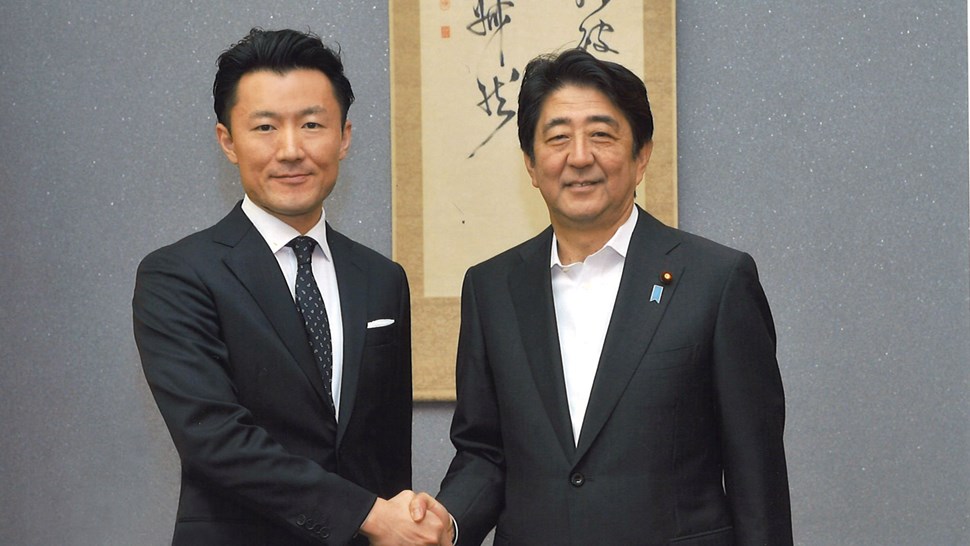
Andrea Chiarello, Head of EU Government Affairs for Pfizer
Some countries have acted in their national legislatures. The German Ministry of Health, for instance, recently announced it was deregulating prices for reserve antibiotics.
The question is how the EU will tackle the issue at a regional level. It is complicated. Production costs in Europe are already high. Hence generic ingredients and drug manufacturing have increasingly migrated to Asia, where costs are lower. How can Europe safeguard its supply of key medicines while still keeping them affordable and globally competitive?
Challenge 2: Creating the Incentives to Spur Innovation and R&D
A longer-term challenge for the EU: How can it create effective incentives for companies to develop new antibiotics and other life-saving medicines? To tackle other diseases, governments and NGOs have experimented with a number of options, from offering financial support up front, tax credits, or lump-sum payments upon approval.
Pfizer’s Andrea Chiarello believes that for antimicrobials, “a package of incentives” is needed. These incentives would have “different but complementary roles: ‘push’ incentives to de-risk early research and ‘pull’ incentives to reward successful development of priority innovative antimicrobials. Country-specific valuation and reimbursement reforms are also required to ensure antimicrobials are adequately valued, remain available on the market, and are accessible to patients.”
A particularly encouraging “pull” incentive that has emerged for antibiotics: transferable exclusivity vouchers, or TEVs (also called TEEs, for transferable exclusivity extensions).
Here’s how they’d work: When a pharmaceutical company developed a new antibiotic that met certain efficacy targets, it could apply for a TEV from the government. That TEV would enable the company to extend the data exclusivity of another one of its products for a period of time (usually between 1 to 5 years). The TEV can also be sold or transferred to another company, which could use the TV to extend the exclusivity of one of its own products. This would allow companies to recoup some of the costs of developing a new antibiotic without relying solely on government funding.

David Earnshaw, Associate Vice President, European Public Policy, MSD [Merck, Sharpe and Dohme]
MSD’s David Earnshaw told Brunswick that TEVs are “one of the policy solutionswhich at last is being suggested as a way to replenish the antibiotic pipeline.This is probably the only solution which is likely to generate a sufficient incentive for R&D in this area.And to be honest, every other approach has failed.”
Public health NGOs and EU member states are less enthusiastic about TEVs. They argue it could delay cheaper competition for some of the most expensive medicines.
Yet Earnshaw believes TEVs represent the most promising, workable solution. “If we are to address the challenge of AMR, we need more antibiotics in developmentand thisis exactly the problem thattheTEV could solvebyencouragingthe development of antibiotics,” he said. “A transferable exclusivity voucher effectively adapts 15thcentury intellectual property rules to 21st century market failure. It is thepolicy solution most likely tobe capable ofreplenishingthe antibiotic pipeline.While this won’t happen overnight, in any case the evidence suggests that it won’t happen at all without the incentive offered by the TEV.”
The Critical Role of Education
Better education and awareness will help both challenges. Helping healthcare providers and patients grasp the importance of antibiotics being used selectively—and correctly—will help minimize their use, thereby shoring up supplies. And as people better appreciate the threat that AMR poses—who wants to live through another pandemic?—it will help garner the public support to make the necessary investments and policy changes to encourage the next generation of antibiotics.
The Opportunity: Respond to the Current Crisis, Deliver on Long-Term Strategy
Much is at stake as the European Commission gets set to review the EU’s pharmaceutical legislation. Mirroring the magnitude of the challenges are the opportunities of overcoming them. Europe has the chance to not only respond to the current crisis, but also put in place a system that helps obviate future ones. Incentivizing antibiotic innovation promises to address a dramatic threat to public health and help Europe’s pharmaceutical industry deliver on the EU’s ambition to be self-reliant and innovative. Even more, it can ensure Europe plays a leading role in helping antibiotics remain one of medicine’s greatest success stories, rather than watching it become one of its great tragedies.