Founded by England’s former Chief Medical Officer, The Trinity Challenge is engineering a collaboration between health, technology and data, for the benefit of mankind.
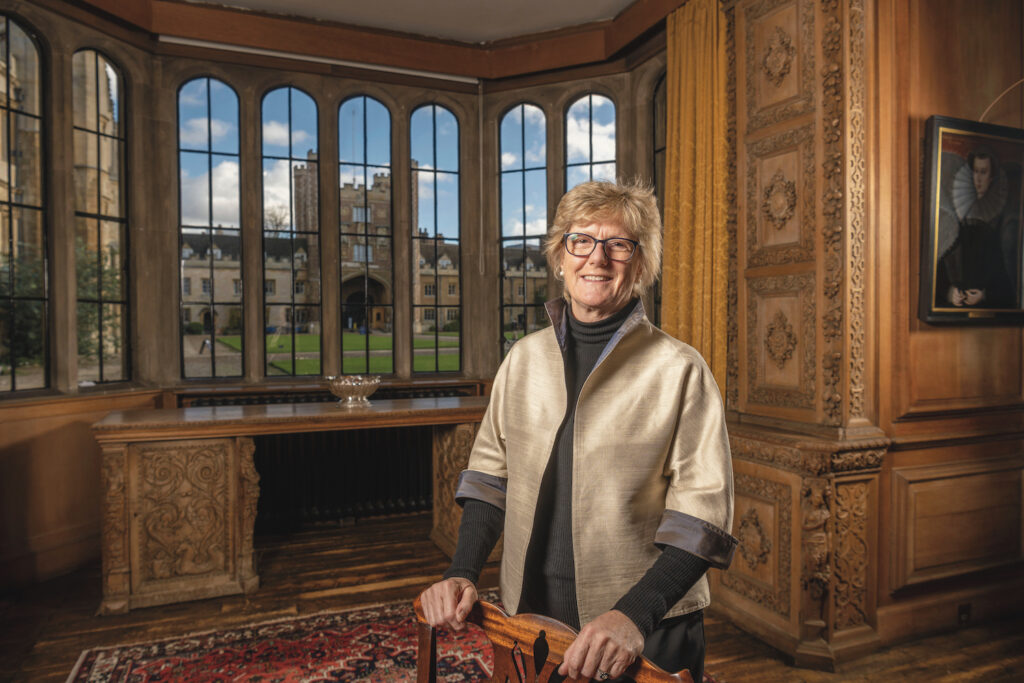
Professor Dame Sally Davies could have stepped back from the front lines of medicine when, after nine years as England’s Chief Medical Officer, she was appointed to serve as Master of Trinity College, Cambridge. Now, the medical leader who had led Britain’s fight against Ebola and other pandemics at home and abroad, and who had taken a global leadership role in the ongoing fight against Anti-microbial Resistance (AMR), could focus on scholarship and collegiate matters. Right?
Hardly. To call Davies driven would be something of an understatement. As the first woman to have held either of these posts, “I’ve always had to be the best to get the jobs,” Davies says in an interview with the Brunswick Review. “As women, we are often told that we can’t do something and we’re rebuffed. I’ve learned not to take it personally, but to come back the next day and try again.”
Her drive has led her toward ever-larger stages. As a clinical hematologist, she was the first UK physician to specialize in sickle cell disease. During her time with the National Health Service, she lobbied for and won the funding to create the National Institute for Health Research, now a world-renowned medical research body with an annual budget of over £1.3 billion. It transformed scientific and medical research in the country, and if that isn’t enough, she has driven reforms and innovations in global health through her role as the UK’s Special Envoy on AMR.
Soon after her arrival in Cambridge, COVID-19 emerged, proving that viral agents of mass destruction pay no attention to national borders.
“As the pandemic set off, I was aware that we were not able to access all the data that policymakers needed to inform their decision making,” she says. “And I was very keen that we should move forward and make a contribution.”
Recognizing the gaps in the data ecosystem made Davies realize that data, analytics and data science had key roles to play. In an effort to harness technology from all corners of the globe, Davies convened a coalition of 42 of the most renowned public, private, philanthropic and academic organizations, including the University of Cambridge, Tencent, Bluedot, Facebook, GSK, Microsoft and Brunswick Group. This marked the founding of The Trinity Challenge (TTC).
In the autumn of 2020, TTC launched a global competition inviting research teams from around the world to enter, aiming to find scalable technologies that could help the world identify, respond to and facilitate recovery from infectious disease outbreaks.
By medical research standards, the prize fund—£6 million—was extremely modest. For comparison, the US put up $18 billion to spur the creation of a COVID-19 vaccine. But the organizations behind Davies’ effort were devoting more than just funding to the cause—they were lending expertise and mentoring as well as access to technology.
With such incentives, it is hardly surprising that the response was extraordinary, and TTC received 340 applications from 62 countries. In June last year, an expert panel of judges selected eight winners whose solutions focused on, or were based in, countries such as Nigeria, Thailand and India.
“I thought of a challenge mechanism because if it is run effectively, it can really stimulate innovation and different thinking. Look at Blood Counts, our second-prize winners. They are mathematicians, and they may never have thought of developing their solution if we hadn’t held the Challenge. They are using their ‘maths brains’ through AI, to interrogate the data held in laboratory ‘boxes’ that do full blood counts, and we now know that there are COVID-19 signatures,” Davies says.
To harness technology from across the globe, Davies convened a coalition of 42 renowned organizations, including University of Cambridge, Facebook, Microsoft and Brunswick Group.
One of five third-place winners, a nonprofit called Living Goods, operates in Burkina Faso, Ethiopia, Kenya and Uganda. As Living Goods explained in their application, the COVID-19 pandemic has shown that interruptions in access to essential services puts children at greater risk of dying from diseases such as malaria, diarrhea
and pneumonia.
Davies concurs as COVID-19, SARS, Ebola, MERS and H1N1 have demonstrated, without strengthened and proactive strategies, global health threats will emerge more often, spread more rapidly, take more lives, disrupt more livelihoods and more greatly impact the world. This points directly to the health concerns of the world’s poorest communities.
Where pandemic preparedness can make the most difference is in ensuring that large segments of the world’s population are not left ill-equipped to cope when pandemics strike.
The TTC’s grand prize winner is the Participatory One Health Disease Detection, or PODD, a Thailand-based organization that turns farmers into disease detectives, to serve as a front-line surveillance system to prevent the spread of diseases jumping from animals to humans.
“The idea is simple,” Davies says. “A mobile phone can be used to ping and tell local health authorities that you have a sick or dead animal. They then check it out, find out what the problem is, and separate it from the rest of the herd. And then map that data with human infections going into the health system.”
The platform already has a network of 20,000 farmers, and with the help of the £1.3 million in prize funding from the TTC, PODD is hoping to expand operations to Cambodia, India, Indonesia, Laos, Uganda and Vietnam over the next three years. A Brunswick Group-TTC podcasts series celebrating the winners is available on Spotify.
In leading the creation of TTC, Davies identified that data and innovation would be catalytic in accelerating diagnoses, analyses and reporting, as well as providing policymakers with vital information needed to make effective decisions. There was also a clear understanding that the private sector would make a crucial contribution to these efforts through its access to unique, large-scale datasets and its comprehensive infrastructure.
“The private sector holds datasets that no one else has,” Davies says, “particularly the big tech platforms. They bring some of the best data architecture and data analysis techniques. We have a need, and they want to help.”
A relationship TTC facilitated between Google and Kushi Health, based in India, is one example. Kushi Health’s digital platform empowers community health workers to screen, refer and follow up with people at a higher risk of death from COVID-19. Google provided access to some of its data to help Kushi Health understand the potential scale of the problem and identify the groups most in need of help. Working with some of the best data architects and analysts in the world has allowed Kushi Health to develop different perspectives to increase the ease with which data could be collected, layered and shared, while protecting privacy.
Davies is also insistent that there needs to be greater global investment in longer-term pandemic prevention. She continues to look ahead, to scaling up global efforts to prevent more lethal infectious disease outbreaks that could be even more profoundly damaging to human security.
Preventing a disease and minimizing its damage doesn’t generate the same attention as the invention of a vaccine. But the value to mankind can be just as dramatic, and already, some of TTC’s winning projects are contributing to pandemic response and resilience efforts, and helping to avoid a repetition of the catastrophic damage inflicted by COVID-19, says Davies, adding, “I think The Trinity Challenge has been an amazing success.”
You can’t sit in a high-income country and understand the best solution for low-income countries. We need Thailand telling us what they need and how they would do it.
Davies gives credit in particular to TTC members, such as Google and the Global Virome Project, which supported applicants’ efforts to refine and build their projects. Such companies shared datasets that were years, even decades, in the making, and also provided mentorship to help applicants assess baselines and grow without becoming overstretched.
Underpinning TTC’s approach has been a recognition of the important role that diversity plays. Global health solutions and innovations are most effective when they are diverse, and arise in the communities that need and will benefit from them the most. They must be developed by those who understand the issues on the ground, the strategies to combat them, and the behavioral and cultural nuances that could affect the uptake or roll-out of new tools.
“How can we know, in the Global North, what is needed in the Global South?” Davies says. “You can’t sit in a high-income country and understand the best solution for low-income countries. We need Thailand telling us what they need and how they would do it.”
Looking back over the past year, the first challenge has convinced Davies of the tremendous value of facilitating collaborations between entrepreneurs, NGOs and the public and private sectors. “I think we will see more public-private partnerships around pandemics, around vaccines, around many things in the global health field,” she says.
Although companies around the world mobilized collectively in the battle against COVID-19, Davies says, “We need to ‘bake in’ these technological advances into the health sector, and we also need to develop our systems so that the behaviors that we’ve built now—the ‘muscle memory’—is not lost. These problems are not going to be solved overnight. We have to work at them, and it starts with mutual respect and understanding and open communication. There is a lot left to do.”
Attention global researchers and funders: Davies and TTC’s coalition members are already considering the scope and structure of the next Challenge, and the topics it may include.
“What we have shown is that surveillance, particularly in low-income countries, is not yet good enough. One option would be to fund regional competitions. We’re trying to craft the next Challenge to deliver the most innovation for the world.”
Areas of interest for TTC include logistics. “Logistics firms have a lot to offer. We need to think about the security of our supply chains for drugs and vaccines, where we are manufacturing them and how we are going to have a system which can really ramp up faster in the future. And of course there is AMR, the ‘Other Pandemic’; I would like to see a Challenge on this topic.”
Davies continues: “And I’d also invite people to join us, whether they are companies or philanthropists who can contribute money or data. You can make a difference and have fun doing it. This has been such fun meeting all the people and helping them realize their dreams.”
—
Abigail Scarlett is an Associate and Emily Thompson is an Executive, both based in Brunswick’s London office, and are members of the Foundations and Non-Profits team.
More from this issue

Acceleration
Most read from this issue
The Wizard of Ads